Nursing Care and Pathophysiology for Heart Failure (CHF)
Included In This Lesson
Study Tools For Nursing Care and Pathophysiology for Heart Failure (CHF)
Outline
Pathophysiology: In heart failure, the heart does not pump effectively. This can occur because of many reasons but usually, because there has been damage to the heart tissue. The heart is not able to pump enough fluid forward so fluid then backs up. This fluid backup increases work on the heart as it tries to keep up and cannot.
Overview
The heart is a pump, circulates blood throughout the body. Heart failure = pump failure. Heart failure occurs when the heart cannot pump enough blood to supply the body’s needs.
Nursing Points
General
- Pump Failure
- Decreased perfusion forwards
- Increased congestion backwards
- Causes
- Myocardial Infarction
- Dead muscle can’t pump
- Hypertension
- ↑ afterload = ↑ stress on heart muscle
- Valve Disorders
- Blood not moving in right direction
- Inefficient pump
- Myocardial Infarction
- Diagnostics
- BNP (Brain Natriuretic Peptide) – stretch of LV
- Echocardiogram
- Ejection Fraction
- Can diagnose valve disorder
- Chest X-Ray (CXR
- Cardiomegaly
- Pulmonary Edema
- Complications
- Volume Overload
- Pulmonary Edema
- Exacerbations
- Decreased Perfusion
- Heart
- Angina, MI
- Arrhythmias
- Organs
- Impaired Kidney Function
- Heart
- Volume Overload
Assessment
- Right-Sided Heart Failure
- Decreased Pulmonary Perfusion
- ↓ oxygenation
- ↓ activity tolerance
- Increased Systematic Congestion
- Peripheral Edema
- ↑ JVD
- ↑ Preload
- Weight Gain
- Fatigue
- Liver / GI Congestion
- Decreased Pulmonary Perfusion
- Left Sided Heart Failure
- Decreased Systemic Perfusion
- Skin pale or dusky
- ↓ Peripheral pulses
- Slow capillary refill
- ↓ renal perfusion
- ↓ urine output
- Kidney Injury / Failure
- Increased Pulmonary Congestion
- Pulmonary edema
- Cough
- Pink/frothy sputum
- Crackles
- Wheezes
- Tachypnea
- SOB on Exertion
- Anxiety/restlessness
- Pulmonary edema
- Decreased Systemic Perfusion
Therapeutic Management
Goal is to decrease workload on heart while still increasing cardiac output. Discussed in more detail in Therapeutic Management Lesson
- Decrease Preload
- Decrease Afterload
- Increase Contractility
Patient Education
Discussed in more detail in Therapeutic Management Lesson
- Diet & Lifestyle Changes
- Medication Instructions
- Activity Restrictions
- Frequent Follow-Ups
ADPIE Related Lessons
Related Nursing Process (ADPIE) Lessons for Nursing Care and Pathophysiology for Heart Failure (CHF)
Transcript
This lesson is going to cover the basics of heart failure.
Heart disease is one of the leading causes of death in the US so you will see Heart Failure quite frequently in clinical practice. We want you to get an Ah-hah moment here and really understand this stuff. We’re gonna give you the most important things you need to know.
So, what exactly causes heart failure? Well remember it’s just pump failure – so anything that impacts the heart’s ability to pump efficiently can cause heart failure.
The top two causes are MI’s and hypertension, but valve disorders can cause a lot of problems, too. So what happens here? Well in an MI, if you remember from those lessons, blood supply is cut off to the heart muscle and the muscle itself dies. Muscle that is dead can’t contract, so the pumping ability or contractility of the heart is affected. Hypertension causes an increased afterload – remember from the hemodynamics lesson.
The heart has to pump harder against a higher pressure in the vessels. After a while, it can get worn out. Ultimately the ventricles can’t efficiently pump against that pressure any more. Someone with valve disorders, like stenosis or regurgitation, will have issues getting the blood where it’s supposed to be. If it’s not going where it’s supposed to, then it’s backing up – causing increased congestion or stretch or preload in the heart. This stress on the heart can lead to heart failure. So again, anything that impacts the heart’s ability to pump efficiently can cause heart failure – this means anything that affect the heart muscle.
BNP Heart Failure Guidelines
So there are multiple ways that we can diagnose and classify heart failure, but we just want you to know these three. The lab value we use is called Brain Natriuretic Peptide or BNP – this is released whenever the ventricles are stretched. So in Congestive Heart Failure patients when they’re severely volume overloaded, we can see this number jump into the thousands. In the labs course we will talk in much more detail about this value, so be sure to check that out.
Heart Failure Chest X-Ray

We’ll also do a chest x-ray, which could show a couple things. You may see the heart is actually enlarged because of the overload and stretch in the ventricles – and you may also see fluid in the lungs – that’s the pulmonary edema. We’ll also get an echocardiogram which can tell us things like end-diastolic volumes (remember that measures preload), ejection fraction, which is usually less than 50% in heart failure, and whether or not there are any valve issues.
Clinical Signs of Heart Failure
So let’s look at what this patient looks like when you actually see them in practice…
In the module intro we asked y’all to brainstorm what you thought this patient looked like. Guys if you get nothing else about Heart Failure, THIS is the part you’ve got to get.
Remember we said that there’s decreased perfusion forward and increased congestion backwards, right? So in right-sided heart failure we’re going to see some oxygenation problems because of decreased perfusion to the lungs. They may struggle with activity because they just don’t have enough blood flow for their lungs!
Then backwards we see that congestion into the system – they are way overloaded in the systemic circulation – so what does that mean? That means peripheral edema – okay how would you feel if you swelled up like crazy? You’d be tired, you’d probably gain some weight? Some of that fluid may even collect in the gut and make you nauseous.
Then because the blood can’t get past the heart from the body, it even backs up into the neck and you’ll see this crazy jugular venous distention – it looks like a rope on their neck!! So if you’re seeing these signs of excessive volume out in the body – you gotta think right sided heart failure!
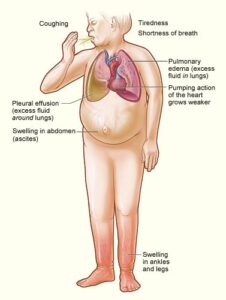
Okay, so what about the left? Well they actually have decreased perfusion to the body. Remember your signs of decreased perfusion? They’re gonna be pale, decreased pulses, maybe slow cap refill, and their skin might even be cold, right? Signs of decreased perfusion. Then, we see the congestion happening in their lungs – y’all their lungs are full of fluid! How would you feel? You’d be struggling to breathe, right? They’ll have a cough, and their sputum will be pink and frothy because there’s just so much blood pumping through the lungs! Imagine if this was you and had all this fluid in your lungs – what position would you want to be in? You lay down and you’ll feel like you’re drowning – a lot of these patients sleep with lots of pillows or even in a recliner. Some of them even lose weight because it becomes a choice to either eat or breathe! So if you see these severe respiratory issues and fluid on the lungs, you’ve got to think Left-sided heart failure!
So right sided the classic sign is the systemic overload and left-sided classic sign is pulmonary edema. If you get this you can pick out any issues they’ll have!
Complications of Heart Failure
Now, there are quite a few other complications of heart failure, but the one I really want y’all to understand is what happens when the kidneys don’t get perfused. So here’s our heart failure patient who has decreased perfusion forward and increased congestion backward. They’re volume overloaded, probably struggling to breathe, and now, they aren’t perfusing their kidneys.
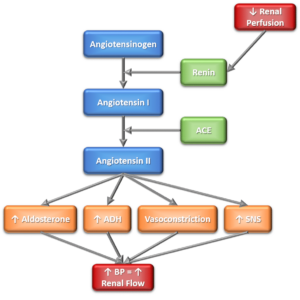
When the kidneys lose blood flow, it stimulates the Renin-Angiotensin-Aldosterone system (RAAS). You will learn more about this in pharmacology, but what you need to know is that it causes three main things to happen in the body.
- The first is water retention because of aldosterone and ADH. The kidneys see a lack of flow and think they need to hold onto water! So it is increasing the preload (or stretch) on ventricles whose preload is already sky-high!
- The second is vasoconstriction. This is the body trying to pull blood towards the heart to increase the blood pressure – this increases afterload (the force the heart has to pump against) – in a patient whose heart is already struggling as it is!
- And the third is the RAAS activates the Sympathetic Nervous System – it’s basically telling the heart to work harder and faster – which it cannot do! The end result is MORE volume overload, MORE stress on the heart muscle, and a perpetuated cycle that never ends.
That’s why I call it the cycle of death. What you’ll see when we look at therapeutic management in the next lesson is that the majority of therapy is aimed at breaking this cycle.
So let’s recap – anything that can affect the heart’s ability to pump effectively can cause heart failure, including an MI, hypertension, and valve disorders. Right-sided heart failure presents with symptoms of decreased pulmonary perfusion and increased systemic congestion – so they’re swollen, gain weight, lots of edema. Left-sided is the opposite – decreased systemic perfusion and increased pulmonary congestion, so these patients are really struggling to breathe. We diagnose with a BNP, Chest X-ray, and Echocardiogram. And don’t forget that the impact this has on the kidneys can make the problem worse – we’ll talk about how we work to break that cycle of death for these patients.
I hope we’ve been able to clear this up for you a bit, like we said sometimes heart failure is overcomplicated! Our goal is to make it easier to understand to give you that peace of mind and confidence! So go out and be your absolute best self today and, as always, happy nursing!
Study Plan for Study Skills, Test Taking for the NCLEX® Using Med-Surg (Lewis 10th ed.) designed for Westmoreland County Community College
Concepts Covered:
- Concepts of Population Health
- Factors Influencing Community Health
- Community Health Overview
- Substance Abuse Disorders
- Upper GI Disorders
- Renal Disorders
- Newborn Care
- Integumentary Disorders
- Tissues and Glands
- Central Nervous System Disorders – Brain
- Digestive System
- Urinary Disorders
- Urinary System
- Musculoskeletal Trauma
- Concepts of Mental Health
- Health & Stress
- Developmental Theories
- Fundamentals of Emergency Nursing
- Communication
- Basics of NCLEX
- Test Taking Strategies
- Prioritization
- Delegation
- Emotions and Motivation
- Integumentary Disorders
- Legal and Ethical Issues
- Basic
- Preoperative Nursing
- Labor and Delivery
- Fetal Development
- Newborn Complications
- Postpartum Complications
- Postpartum Care
- Labor Complications
- Pregnancy Risks
- Prenatal Concepts
- Circulatory System
- Cardiac Disorders
- Emergency Care of the Cardiac Patient
- Vascular Disorders
- Shock
- Postoperative Nursing
- Intraoperative Nursing
- Oncology Disorders
- Neurological Emergencies
- Respiratory Disorders
- Female Reproductive Disorders
- Acute & Chronic Renal Disorders
- Liver & Gallbladder Disorders
- Lower GI Disorders
- Disorders of Pancreas
- Disorders of the Thyroid & Parathyroid Glands
- Disorders of the Adrenal Gland
- Disorders of the Posterior Pituitary Gland
- Immunological Disorders
- Hematologic Disorders
- EENT Disorders
- Integumentary Important Points
- Musculoskeletal Disorders
- Emergency Care of the Neurological Patient
- Peripheral Nervous System Disorders
- Central Nervous System Disorders – Spinal Cord
- Neurologic and Cognitive Disorders
- Eating Disorders
- Noninfectious Respiratory Disorder
- Respiratory Emergencies
- Infectious Respiratory Disorder
- Psychological Emergencies
- Trauma-Stress Disorders
- Personality Disorders
- Cognitive Disorders
- Bipolar Disorders
- Depressive Disorders
- Psychotic Disorders
- Anxiety Disorders
- Somatoform Disorders
- Infectious Disease Disorders
- Musculoskeletal Disorders
- Renal and Urinary Disorders
- Cardiovascular Disorders
- EENT Disorders
- Gastrointestinal Disorders
- Hematologic Disorders
- Oncologic Disorders
- Endocrine and Metabolic Disorders
- Childhood Growth and Development
- Adulthood Growth and Development
- Medication Administration
- Nervous System
- Dosage Calculations
- Learning Pharmacology
- Prefixes
- Suffixes

