Nursing Care and Pathophysiology of Acute Kidney (Renal) Injury (AKI)
Included In This Lesson
Study Tools For Nursing Care and Pathophysiology of Acute Kidney (Renal) Injury (AKI)
Outline
Overview
- Sudden onset renal damage
- Loss of renal function due to poor circulation or renal cell damage
- Usually reversible may resolve on its own
- Can lead to permanent damage if not reversed quickly
Pathophysiology
Sudden decline in the function of the kidneys usually from decreased blood flow to the kidneys or injury to the kidney from inflammation and toxins. Acute kidney injury can be reversed if diagnosed and treated early but can progress to renal failure.
Nursing Points
General
- Causes
- Prerenal: decreased blood flow to kidneys, accounts for majority of cases
- Hypotension
- Hypovolemia
- ↓ Cardiac Output (i.e. Heart Failure, Shock)
- Intrarenal: damage within the kidney itself
- Tubular necrosis
- Infection
- Obstruction
- Contrast dye
- Nephrotoxic medications
- Postrenal: damage between the kidney and urethral meatus backs up, causing damage to kidneys
- Infection
- Calculi
- Obstruction
- Prerenal: decreased blood flow to kidneys, accounts for majority of cases
- Phases
- Onset
- Note a decrease in baseline urine output
- Oliguric
- Decreased urine output <400 mL/day
- Sickest phase
- ↑ BUN/Creatinine
- ↓ Glomerular Filtration Rate (GFR)
- Diuretic
- Beginning to recover
- Gradual urine output increase followed by diuresis
- Recovery
- Decreased edema
- Electrolytes normalize
- GFR increases
- Onset
Assessment
- Signs and symptoms result from kidneys inability to regulate fluid and electrolytes
- Azotemia (retention of nitrogen wastes in blood)
- ↑ BUN/Creatinine
- ↓ Glomerular Filtration Rate (GFR)
- Decreased urine output in oliguric phase
- Should see increase in diuretic phase
- Signs of volume overload (HTN, peripheral edema, pulmonary edema)
- s/s infection if that was the source
- Metabolic acidosis
- Kidneys not holding HCO3–
- Electrolyte abnormalities
- ↑ Potassium
- ↓ Sodium
- ↑ Phosphate
- ↓ Calcium
Therapeutic Management
- Oliguric Phase
- Restrict fluid intake
- Identify & treat cause
- Diuretics
- Diuretic Phase
- Replace fluids and electrolytes
- Especially watch K+ & Na+ levels
- Replace fluids and electrolytes
- If not recovering, may need dialysis
Nursing Concepts
- Fluid & Electrolyte Balance
- Daily weights
- Strict I&O
- Monitor electrolytes and replace as needed
- Fluid restriction in oliguric phase
- Elimination
- Monitor urine output
- Normal = >30mL/hr
- Look for progression from oliguric to diuretic phase
- Monitor for s/s UTI
- Prepare patient for dialysis
- Monitor urine output
Patient Education
- Avoid foods high in sodium or potassium
- Caution – salt substitutes made with potassium chloride
- Educate on fluid restriction
- s/s to report to nurse or provider, especially chest pain
ADPIE Related Lessons
Related Nursing Process (ADPIE) Lessons for Nursing Care and Pathophysiology of Acute Kidney (Renal) Injury (AKI)
Transcript
In this lesson we’re going to talk about acute kidney injury. As you can guess, this is when we have a sudden onset of kidney damage and the kidneys get injured acutely.
Acute Kidney Injury is a sudden loss of renal function.
It’s generally caused by a perfusion issue or damage to the kidney tissue itself.
You can see the bleeding and swelling within this kidney that has been damaged. You can imagine how hard it would be for a kidney with this kind of damage to do its job, right? Now, it’s usually reversible or resolves on its own in a week or two.
It can also be prevented, so think about that when we look at the causes here in a second. If we aren’t able to reverse it or it doesn’t resolve quickly, it can lead to permanent damage and cause the patient to develop Chronic Kidney Disease, or CKD, which we’ll talk about in the next module.

Causes of Acute Kidney Injury (AKI)
There are three categories of causes of acute kidney injury and it all has to do with the source of the problem.
- Prerenal
- Intrarenal
- Postrenal
Prerenal
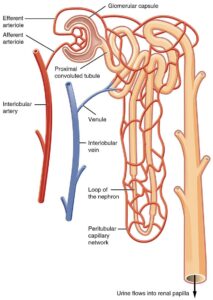
So prerenal, pre means before, so the source of the problem is what comes before the kidneys – which means the blood flow into the kidneys. If blood isn’t flowing into the kidneys, not only do they not get perfused and can incur some ischemic damage, but they also can’t filter the blood if it’s not there, right? Some causes of prerenal kidney injury include hypotension, hypovolemia, or any decrease in cardiac output like heart failure or shock.
Intrarenal
Intrarenal means that the source of the problem is coming from within the kidneys themselves – so the blood flow is fine, but there’s been damage to the kidney tissues or cells that are making it not work correctly. Common causes of intrarenal kidney injury are infection, tubular necrosis, nephrotoxic drugs, or damage from contrast dye. That contrast dye is concentrated and sometimes hard to filter out of the kidneys. That’s why you’ll see us give patients extra fluids before they get a contrast scan to help protect the kidneys.
Postrenal
And finally postrenal, as you can guess, is caused by something happening after the kidneys. What usually happens is there’s some sort of infection or obstruction like a stone that causes backflow into the kidneys. The kidneys fill with that fluid because it can’t get out – that’s called hydronephrosis – and it causes damage and decreased kidney function.
So ultimately prerenal and postrenal sources will cause damage to the kidney itself, but we name this based on the original source of the problem. You can also see how a lot of this is preventable – we need to make sure we keep the patient’s blood pressure up, we need to keep them well hydrated, we need to protect their kidneys from damage with those drugs or contrast, and we need to treat infections and remove obstructions as quickly as possible.
Phases of Acute Kidney Injury
So, let’s talk phases – acute kidney injury goes through 4 phases. You really want to try to catch this as early as possible! In onset, what happens is we start seeing a decline in their baseline urine output. Well you know what we want as our minimum is about 30 mL/hr, right? That’s about 720 mL/day. What will happen is they’ll be cruising along at 1200 mL a day, about 50 mL/hr and you’ll notice it goes down to about 30 mL/hr. And you’ll think…no worries, it’s still above that minimum, right? But they actually just dropped their baseline urine output by almost 500 mL a day! Notice these things, guys! Trends are important. So, then as they continue to get worse, they’ll drop into what’s known as the Oliguric phase – this is the acute, sick phase of acute kidney injury, We’ll see their urine output drop to less than 400 mL/day (that’s like 16 mL/hr) and what urine they do produce will be concentrated and dark. Their BUN and Creatinine will start to go up because the kidneys aren’t doing their job, and we’ll see our GFR, or our glomerular filtration rate, drop – because the kidneys aren’t filtering the blood as fast as they should. During this phase, we’re going to see all the symptoms of kidney failure that we’ll talk about in just a second. As their kidneys begin to recover, they’ll move into the diuretic phase. We’ll see their urine output slowly increase and then suddenly they’ll start diuresing like crazy – basically now that their kidneys are working, they’re trying to get rid of all the fluid they’ve been holding onto. Then, when patients get into the recovery phase, we see our GFR normalize and slowly but surely everything brings itself back into alignment.
Symptoms of Oliguria
So, what symptoms are we going to see during that oliguric phase? Well all the symptoms are based on the fact that the kidneys are unable to perform their normal functions. We talked about those in detail in the module intro. So we see azotemia, which is a buildup of nitrogenous waste products, since they can’t filter them out – that’s when we see the BUN and Creatinine elevate.
We see their GFR drop – now I want to stop here because GFR isn’t given enough credit in nursing school – ask anyone what labs they check for the kidneys and they say BUN & creatinine! But – did you know that both BUN and Creatinine can be elevated for other reasons like dehydration or muscle damage? BUT – the GFR literally measures the amount of volume the glomerulus in our kidneys can filter in any given minute. It is highly specific to the kidneys and highly reflective of kidney function! Don’t discount it!
That being said – we already talked about seeing a decrease in urine output and how concentrated it would be. Since they aren’t able to get that fluid out, we actually start to see signs of volume overload in their system. We’ll see significant peripheral edema, and as it progresses, we begin to see pulmonary edema as well – so you’ll hear crackles and they’ll get short of breath.
Because the kidneys aren’t retaining that bicarb buffer like they should, we can see metabolic acidosis. That’s a pH less than 7.35 and a HCO3- less than 22. And we know that non-functioning kidneys can’t regulate electrolytes. We’ll look at this more closely in chronic kidney disease, but what we’ll see is an increased potassium, decreased sodium, increased phosphate, and decreased calcium. And then, of course, if infection was the source, we may see signs of infection.
So what do we do? Well during the oliguric phase, we try to restrict fluids a bit. The last thing we need to do is overload them even more than they already are. We want to work to identify and treat the cause and we’ll give diuretics to get that fluid off. Once they hit the diuretic phase, we want to make sure we balance their fluid status and replace any electrolytes as needed. We especially want to watch potassium and sodium because those can be life threatening if they’re outside of their normal range. If patients don’t seem to be getting better or aren’t responding to treatment, we may need to start them on hemodialysis. We’ll talk more about hemodialysis in the next module.
Nursing Care Plan for Acute Kidney Injury
Our priority nursing concepts for a patient with acute kidney injury are obviously fluid & electrolytes and elimination, but also perfusion because we want to make sure their kidneys are getting the blood flow that they need. Make sure you check out the care plan attached to this lesson for more detailed nursing interventions and rationales.
So let’s recap quickly. Acute kidney injury is sudden onset kidney damage that can be preventable and is usually reversible if caught early enough. We work to identify and treat the cause (whether it’s prerenal, intrarenal, or postrenal) as quickly as possible before permanent damage is done. We’ll see signs of volume overload and electrolyte abnormalities, as well as things like azotemia and metabolic acidosis that tell us the kidneys aren’t doing their job. We want to support those kidney functions by giving electrolytes or bicarb as needed, as well as diuretics, and we know that the patient may require dialysis if they aren’t recovering well.
So that’s it for Acute Kidney Injury, make sure you check out the resources attached to this lesson, as well as the rest of the lessons within this module to learn more. Now, go out and be your best self today. And, as always, Happy nursing!
Study Plan for Study Skills, Test Taking for the NCLEX® Using Med-Surg (Lewis 10th ed.) designed for Westmoreland County Community College
Concepts Covered:
- Concepts of Population Health
- Factors Influencing Community Health
- Community Health Overview
- Substance Abuse Disorders
- Upper GI Disorders
- Renal Disorders
- Newborn Care
- Integumentary Disorders
- Tissues and Glands
- Central Nervous System Disorders – Brain
- Digestive System
- Urinary Disorders
- Urinary System
- Musculoskeletal Trauma
- Concepts of Mental Health
- Health & Stress
- Developmental Theories
- Fundamentals of Emergency Nursing
- Communication
- Basics of NCLEX
- Test Taking Strategies
- Prioritization
- Delegation
- Emotions and Motivation
- Integumentary Disorders
- Legal and Ethical Issues
- Basic
- Preoperative Nursing
- Labor and Delivery
- Fetal Development
- Newborn Complications
- Postpartum Complications
- Postpartum Care
- Labor Complications
- Pregnancy Risks
- Prenatal Concepts
- Circulatory System
- Cardiac Disorders
- Emergency Care of the Cardiac Patient
- Vascular Disorders
- Shock
- Postoperative Nursing
- Intraoperative Nursing
- Oncology Disorders
- Neurological Emergencies
- Respiratory Disorders
- Female Reproductive Disorders
- Acute & Chronic Renal Disorders
- Liver & Gallbladder Disorders
- Lower GI Disorders
- Disorders of Pancreas
- Disorders of the Thyroid & Parathyroid Glands
- Disorders of the Adrenal Gland
- Disorders of the Posterior Pituitary Gland
- Immunological Disorders
- Hematologic Disorders
- EENT Disorders
- Integumentary Important Points
- Musculoskeletal Disorders
- Emergency Care of the Neurological Patient
- Peripheral Nervous System Disorders
- Central Nervous System Disorders – Spinal Cord
- Neurologic and Cognitive Disorders
- Eating Disorders
- Noninfectious Respiratory Disorder
- Respiratory Emergencies
- Infectious Respiratory Disorder
- Psychological Emergencies
- Trauma-Stress Disorders
- Personality Disorders
- Cognitive Disorders
- Bipolar Disorders
- Depressive Disorders
- Psychotic Disorders
- Anxiety Disorders
- Somatoform Disorders
- Infectious Disease Disorders
- Musculoskeletal Disorders
- Renal and Urinary Disorders
- Cardiovascular Disorders
- EENT Disorders
- Gastrointestinal Disorders
- Hematologic Disorders
- Oncologic Disorders
- Endocrine and Metabolic Disorders
- Childhood Growth and Development
- Adulthood Growth and Development
- Medication Administration
- Nervous System
- Dosage Calculations
- Learning Pharmacology
- Prefixes
- Suffixes
