Atrial Fibrillation (A Fib)
Included In This Lesson
Study Tools For Atrial Fibrillation (A Fib)
Outline
Overview
- Atrial fibrillation
- Multiple disorganized cells produce additional electrical impulse in atria
- Causes atria to quiver at a fast rate
- <300 bpm
- Unable to effectively contract
- Pooling of blood in atria
- High risk for stroke
- AV node blocks some of the electrical impulses from reaching the ventricles
- Rapid irregular ventricular contractions
- Causes atria to quiver at a fast rate
- Multiple disorganized cells produce additional electrical impulse in atria
Nursing Points
General
- Characteristics of Atrial fibrillation
- Rhythm
- Irregular
- Rate
- Atrial rate
- >300 bpm
- Wavy baseline
- Ventricular rate
- 60-100 bpm
- >100 bpm
- “Rapid Ventricular Response” (RVR)
- Atrial rate
- P:QRS ratio
- No obvious P waves
- Wavy baseline
- Not measurable
- No obvious P waves
- PR interval
- Not measurable
- QRS complex
- 0.06-0.12 seconds
- Rhythm
Assessment
- Patient Presentation
- Palpitations
- Fatigue
- Lightheaded/Syncope
- Acute or chronic
- If chronic
- Monitor rate/meds
- If acute
- Convert to NSR
- If chronic
- Atrial and ventricular rates
- RVR
- Decreased Cardiac Output
- Syncope
- Hypotension
- PT/INR
- If taking Coumadin
Therapeutic Management
- Nursing Interventions
- Acute or chronic
- 12 Lead EKG
- Restore NSR
- Assess for s/s of stroke
- Convert to NSR
- Control ventricular rate
- Medications
- Antiarrhythmics
- BB
- Calcium Channel Blockers
- Transesophageal Echocardiogram (TEE) or Cardioversion (CV)
- Ablations
- Medications
- Decreased risk for stroke
- Anticoagulants
- Coumadin (Warfarin)
- Xarelto (Rivaroxaban)
- Eliquis (Apixaban)
- Anticoagulants
Nursing Concepts
- EKG Rhythms
- Perfusion
- Clotting
Patient Education
- Do not miss a dose of on anticoagulants
- Check PT/INR as instructed
- Check radial pulse
- Report if >100
Related Lesson
Transcript
Hey guys, my name is Brad and welcome to nursing.com. And in today’s video, we are going to discuss atrial fibrillation, also known as AFib. I’d like to discuss some of the physiology behind what a-fib actually is, how this might present in a patient, some of the treatment modalities, and most importantly, for this lesson, how to recognize it on an EKG. Let’s dive in.
So in atrial fibrillation, what is occurring is the atria quiver, those top two chambers of the heart, instead of contracting and ejecting blood down into those ventricles, they just kind of quiver. No real conduction occurs, no real contraction occurs. And as a result, blood just sits there, stagnated in those atrium. And the reason why is, we don’t have proper conduction from this SA node, a normal electrical conduction system originates at the SA node, going down to the AV node, through the bundle of His and terminating in those Purkinje fibers. In a-fib we actually have an issue with that SA node. There’s a problem there. And let’s also remember that this electrical conduction system actually resides within the heart muscle itself. This SA node kind of being up here in the right atria. What actually occurs, because we have a dysfunctional SA node, our electrical impulse comes from this atrial tissue itself, and that is problematic. What this essentially occurs, or causes to occur, is a cyclical, electrical impulse to be sent cyclically, circularly all throughout this atrial tissue at a rate of 400 beats per minute. Now let’s recall also from our electrical A and P that this AV node actually acts as a filter. So let’s imagine it’s a filter and we don’t want to allow 400 atrial beats per minute to reach these ventricles because if that were to occur, then we’re basically looking at 400 beats per minute ventricularly. That’s not compatible with life. So this AV node acts as a filter, not allowing all 400 beats per minute to go through. It actually ends up reducing this ventricular rate for about 150 beats per minute. This is important. This is going to be clinically significant whenever we’re actually looking at a-fib.
So what are some causes of atrial fibrillation? Well, this all really kind of comes down to poor perfusion of that heart tissue, right? In instances, such as hypertension, congestive heart failure, coronary artery disease. Essentially, you have to remember guys, this is so crucially important. You have to remember that, that electrical conduction system that we mentioned, it all actually lies right here within this heart muscle itself. So in cases, such as coronary artery disease, where there is a poor perfusion to this heart tissue itself, you have to remember, if there is no perfusion, then there is going to be no conduction. And if there’s no conduction, there’s going to be no contraction, right? You have to remember, not only is that heart muscle responsible for contracting, so if there is an impaired amount of blood being delivered to these heart tissues, you’re not only impairing the muscle itself, but you’re also impairing that electrical conduction system as well. Some assessment findings that we may see in patients who have a-fib are palpitations. Again, an atrial rate of 400 beats per minute, atria just quivering and not quite contracting, a hundred percent going to result in palpitations. You’re going to feel that fluttering in your chest, this fluttering in your chest causes anxiety. This atrial quiver, this impaired electrical conduction system is going to cause shortness of breath, right? Impaired perfusion, impaired electrical conduction system, impaired contraction. If your LV can’t contract effectively to get blood out of the heart, we’re going to end up seeing shortness of breath as a result.
And it’s also important to remember your atrial kick. It’s something that they call an atrial kick, right? This is essentially the kick of blood that comes out of the atria down into the ventricles and the amount of blood that ends up getting ejected out of your ventricles, right? The amount of blood that ends up getting ejected out of these ventricles down here, 30% of that comes from your atria. That’s why, a-fib is so devastating. You’re literally losing 30% of your atrial kick. You’re losing 30% of the blood normally ejected out of the ventricles because instead of properly contracting, these atria are just quivering.
Now some therapeutic management that is important to be mindful of, right? How are we going to treat a patient who is in a-fib whose atria are contracting at 400 beats per minute, and we’re losing that atrial kick of blood, right? Cardioversion. This could be mechanical. This could also be chemical cardioversion being hooking a patient up to that defibrillator machine. And instead of using it to defibrillate them, we can use it to cardiovert them, basically providing a shock to the heart, less joules, less energy than we normally would in cardiac code defibrillating. But a way to try and knock that heart out of that abnormal rhythm. Cardioversion can also be a chemical, right? Antiarrhythmic medications such as amiodarone, right. These are medications used to try and stabilize wild and erratic rhythms. Also medications such as negative chronotropes. Remember chronotropes essentially are medications that affect heart rate and negative chronotropes are responsible for decreasing heart rate. Medications such as, metoprolol, for instance, right, ending in -olol. And then also anticoagulation. This is a big component of the big thing to know with, a-fib, okay. Important, incredibly important because these atria are not contracting. And instead they’re just quivering and blood is just sitting in here, stagnant, not emptying. We’re not getting rid of that atrial kick of 30% of blood, right? Instead it’s just stagnating and sitting there quivering. Stagnant blood clots, guys. So clots can form in these atria. And if these clots were to get ejected through the ventricles and out of the body, this is going to be problematic, right? Pulmonary embolisms strokes, myocardial infarction.
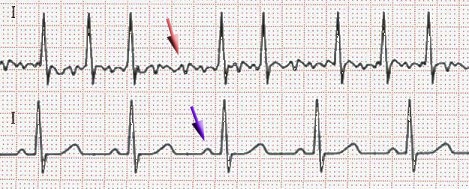
Now using the six step method to solve for a-fib. This is how we’re going to be able to read a-fib on an EKG, right? Our heart rate, remember that atrially, we’re looking at 400 beats per minute and ventricularly, what we should see is approximately 150 beats per minute.
Regularity. That R to R regularity. There will be no regularity at all. It’s going to be completely variable that R to R interval. And this is just due to the rapid nature at which those atria are contracting.
P to QRS interval. The big, important thing that you need to know whenever you’re looking at an AFib on an EKG is that P waves are gone. You can not see P waves and why? Well, again, remember that cyclical nature at which those atrial tissues are firing these electrical impulses off at approximately 400 beats per minute. You’re not able to distinguish a P wave on an EKG due to such rapid firing. And because there’s no P wave identifiable, you can not measure a PR interval.
And then regarding the QRS complex, you’re going to see a normal QRS complex length. Remember it’s 0.06 0.12 seconds. Let’s take a look at an example to bring further clarity.
So if we wanted to take a look at the six step method that we normally would use to solve a-fib and we were taking a look at this one here in particular, as an example, let’s remember, let’s take a look at our heart right now. There’s no real identifiable way to measure an atrial heart rate. It’s just important to know in a-fib. And it’s approximately 400 beats per minute, but let’s take a look at our six seconds strip over here and actually measure our heart rate. Remember how many QRS complexes do we have? And then we multiply that by 10. So 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12 times 10 (12 X 10 = 120) giving us a heart rate of approximately 120 beats per minute. Like I said, we’ve been educating that we look at approximately 150 beats per minute. It’s not always exactly150, as we can see by this example.
Now, the next thing that we want to do is take a look at our R to R interval. Again, we’re actually looking at the R wave and we’re measuring the distance between each individual R wave. And what you will notice is that there’s actually variability here, right? This is much longer in length than this shorter R to R interval again, in a-fib, no actual regularity in the R to R or P to QRS complex ratio. Again, P waves are gone. We cannot see these P waves complete loss of P waves, right? So you cannot measure the P to QRS complex ratio like that. Next thing would be our PR interval. Again, you cannot see a P wave. So we can’t measure a PR interval. That is the big distinguishing factor with a-fib. There’s no P wave and we have a rapid heart rate.
Next thing is our QRS complex. We would actually measure our QRS complex looking at one small square 0.04, two small squares 0.08. So our QRS complex is 0.08 seconds (0.04 X 2 = 0.08), which again, we will remember is normal. And this is the way that we’re going to solve for a-fib. We have a loss of P waves. Our heart rate is approximately 150 beats per minute, no regularity at all with our R to R interval. We are certainly looking at a rhythm that is a-fib.
So to summarize some of our key points with a-fib, it’s important to remember in atrial fibrillation, the atria are just quivering, right? Blood is sitting in there, stagnated. Electrical impulse originating from atrial tissues, instead of the SA node, is just cyclical firing, and then uncoordinated in an uncontrolled manner at approximately 400 beats per minute. And then it eventually is filtered out by that AV node, leaving a ventricular rate of approximately 150 beats per minute. We’re going to recall that there is no regularity. This is a completely uncontrolled firing of impulses from that atrial tissue. It’s uncontrolled. So there’s no regularity at all. Then we’re also going to notice there is a loss of P wave, complete loss of P wave, a big clinical indicator whenever you’re reading EKG. So you’re not going to be able to see one P wave for every QRS, nor are you going to be able to measure a PR interval length. But whenever we take a look at the QRS complex recall, that is indeed going to be identified as normal.
Guys, I really hope that this helps you understand a-fib, not just looking at an EKG test, but also to be able to clinically understand what a patient is experiencing physiologically and how we may be able to treat that patient experiencing AFib. I hope that you guys go out there and be your best selves today. And as always, happy nursing.
Final Exam
Concepts Covered:
- Terminology
- Urinary System
- Respiratory Disorders
- Acute & Chronic Renal Disorders
- Disorders of the Adrenal Gland
- Oncology Disorders
- Integumentary Disorders
- Preoperative Nursing
- Musculoskeletal Trauma
- Integumentary Disorders
- Respiratory Emergencies
- Disorders of the Posterior Pituitary Gland
- Hematologic Disorders
- Renal Disorders
- Labor Complications
- Immunological Disorders
- Upper GI Disorders
- Neurological Emergencies
- Disorders of Pancreas
- Musculoskeletal Disorders
- Cardiac Disorders
- Disorders of the Thyroid & Parathyroid Glands
- Integumentary Important Points
- Pregnancy Risks
- Urinary Disorders
- Vascular Disorders
- Central Nervous System Disorders – Brain
- Nervous System
- Lower GI Disorders
- Intraoperative Nursing
- Eating Disorders
- Circulatory System
- Postoperative Nursing
- Liver & Gallbladder Disorders
- Emergency Care of the Cardiac Patient
- Female Reproductive Disorders
- Shock
- Respiratory System
- Substance Abuse Disorders
- Fetal Development
- Proteins
- Noninfectious Respiratory Disorder
- Newborn Care
- Statistics
- Emergency Care of the Neurological Patient
- Basics of Sociology
- Bipolar Disorders
- Infectious Respiratory Disorder

