Addisons Disease
Included In This Lesson
Study Tools For Addisons Disease
Outline
Pathophysiology:
Addison’s occurs because there is an elevated level of serum ACTH and inadequate amounts of corticosteroids.
Overview
- Hyposecretion of adrenal cortex hormones
- Decreased levels of glucocorticoids and mineralocorticoids leads to
- Electrolyte imbalances
- Decreased vascular volume
- Fatal if untreated
Nursing Points
General
- Adrenal Cortex
- Glucocorticoids
- Cortisol
- Glucose & Fat Metabolism
- Anti-inflammatory
- Mineralocorticoids
- Aldosterone
- Regulate fluid and electrolytes
- Sex hormones (Androgens)
- Testosterone, Estrogen
- Control physical features
- Control hair distribution
- Glucocorticoids
- Adrenal Medulla
- Epinephrine (Adrenaline)
- Norepinephrine (Noradrenaline)
- Fight or Flight Response
Assessment
- Cardiovascular
- Hypotension
- Tachycardia
- Metabolic
- Weight loss
- Integumentary
- Hyperpigmentation (bronzing)
- Electrolytes
- Hyperkalemia
- Hypercalcemia
- Hyponatremia
- Hypoglycemia
- Addisonian Crisis
- Acute exacerbation
- Severe electrolyte disturbance
Therapeutic Management of Addisons Disease
- Replace adrenal hormones
- Corticosteroids
- Hydrocortisone
- Prednisone
- Corticosteroids
- Addisonian Crisis
- Monitor electrolytes and cardiovascular status closely
- Administer adrenal hormones as ordered
- Administer electrolyte replacement as needed
Nursing Concepts
- Fluid & Electrolytes
- Monitor Vital Signs
- Monitor electrolytes (potassium, sodium, calcium)
- Replace electrolytes as needed
- Hormone Regulation
- Administer replacement adrenal hormones as needed
- Lifelong medication therapy needed
- Glucose Metabolism
- Monitor glucose levels
- Treat low blood sugar
Patient Education
- Increase salt and water intake if exercising
- S/s of Addisonian Crisis
- May require increased medication dosing if ill, notify provider
ADPIE Related Lessons
Related Nursing Process (ADPIE) Lessons for Addisons Disease
Transcript
In this lesson we’re going to talk about Addison’s Disease. You’ll see that this is the opposite of Cushing’s Syndrome which we’ll talk about in the next lesson. Addison disease and cushing syndrome involve the adrenal glands.
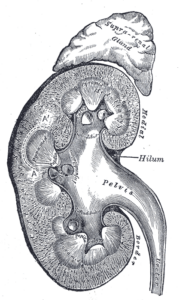
Let’s quickly review the A&P of the adrenal glands. If you can understand what they do, it’s easier to understand what happens when something goes wrong. The adrenal glands sit on top of the kidneys. They have two parts – the outer portion is called the adrenal cortex, the inner portion is the adrenal medulla.
The adrenal cortex is responsible for secreting hormones such as glucocorticoids, mineralocorticoids, and androgens.
Function of the Adrenal Glands
- Glucocorticoids help manage glucose and fat metabolism and have anti-inflammatory properties – they suppress immune response.
- Mineralocorticoids like aldosterone help with fluid & electrolyte balance.
- And androgens are sex hormones like testosterone and estrogen.
The adrenal medulla secretes epinephrine or adrenaline and norepinephrine, or noradrenaline. These hormones are responsible for the fight or flight response in the sympathetic nervous system.
In Addison’s Disease, we see a hyposecretion of hormones, specifically the ones from the adrenal cortex, the outside of the adrenal glands. So that’s decreased glucocorticoids like cortisol, decreased mineralocorticoids like aldosterone, and decreased androgen hormones. Start thinking about what this will look like in your patient.
- Cortisol is responsible for storing fat and it increases glucose levels, so what happens if we don’t have that?
- Aldosterone is responsible for retaining sodium and water, what happens if we don’t have that?
Those effects are going to be seen throughout the body. In the cardiovascular system, we’re going to see hypotension – why? Because there’s not enough aldosterone holding onto fluids – so our intravascular volume goes down. Remember from the hemodynamics lesson that when the blood pressure goes down, the heart rate increases to try to compensate, right? So we see tachycardia as well. Remember that cortisol is responsible for storing fats, so without enough cortisol, we see weight loss.

Patients with Addison’s disease also have this hyperpigmentation or bronzing of the skin. We may even say they have a persistent tan. Sometimes these initial symptoms are ignored – they’ve got tan, they’re losing weight – they won’t recognize that as a bad thing – but then they’ll start to get tired and fatigued from the low blood pressure and that’s when they’ll start to seek help.
Then, since we know that our mineralocorticoids are affected, we’re going to see electrolyte abnormalities. Remember that aldosterone is responsible for retaining sodium and water….so if we don’t have enough, we see sodium levels drop. And any time the kidneys are excreting sodium, they are retaining potassium, so we’re gonna start to see hyperkalemia. Both of these conditions are dangerous for patients because of their effects on the cardiovascular and neurological systems. We’ll also see hypercalcemia – because normally glucocorticoids help bones absorb calcium – and hypoglycemia because the glucocorticoids aren’t present to increase glucose levels. These patients could get quite hypoglycemic, so we need to monitor their sugars closely and treat low blood sugars.
Patients with Addison’s Disease can also have what’s called Addisonian Crisis. This is essentially an acute exacerbation of their disease. We see extreme symptoms, severe hypoglycemia, severe electrolyte abnormalities, and ultimately we can see cardiovascular collapse because of the lack of those hormones. This is a medical emergency, they need to be on a cardiac monitor and likely in an ICU until their condition is under control.
Addison’s Disease Treatment
Now….what kinds of things would we do for them? Well – we know this is a lack of secretion of hormones, right?
So the #1 treatment is to replace those hormones!
Primarily we will give these patients corticosteroids like Prednisone. They may also get mineralocorticoids like Fludrocortisone to help replace the functions of aldosterone. We will also replace their electrolytes as needed, usually this looks like encouraging them to increase their salt and water intake, especially before exercise. These patients will need to be on these medications for the rest of their lives. It can be a big adjustment, but they’ll feel so much better afterwards. This image is the same lady from the previous slide, except after treatment. You can see her cheeks have filled out, she no longer has the hyperpigmentation of her skin, and she just overall looks healthier. She will stay on these medications for the rest of her life.
When we have these patients in the hospital, especially those in Addisonian crisis, we want to monitor their vital signs and EKG closely, monitor their electrolytes, and monitor their blood sugar. We need to make sure we have a plan for treating their blood sugar levels. We’ll talk more about this in the Diabetes lesson, but the general rule when treating a low blood sugar is the 15-15 rule. Give 15g of sugar (Usually juice works great) and re-check in 15 minutes. If they have a decreased LOC and can’t take anything by mouth, we’ll usually give ½ amp or an amp of D50 IV or we could even give glucagon IM to get their sugars up.
Our priority concepts for a patient with Addison’s Disease are going to be Fluid & Electrolytes, Hormone Regulation, and Glucose Metabolism. Make sure you check out the care plan attached to this lesson to see more detailed nursing interventions and rationales.
So let’s do a quick recap. Addison’s disease is hyposecretion of hormones from the adrenal cortex – so decreased glucocorticoids, decreased mineralocorticoids, and decreased androgens. The androgen effects don’t play as much of a role in Addison’s as they do in Cushing’s as you’ll see. We see alterations in their fluid and electrolytes. A decreased vascular volume causes hypotension, they are excreting sodium and retaining potassium, and will have a high calcium and low blood sugar levels. Left untreated, patients can experience cardiac arrhythmias and lead into an acute exacerbation called Addisonian crisis. That leads to severe electrolyte abnormalities and potentially cardiovascular collapse and is an emergent situation. So make sure you advocate to get your patient to a higher level of care if needed.
So those are the basics of Addison’s Disease. Make sure you check out all the resources attached to this lesson to learn more. Now, go out and be your best selves today. And, as always, happy nursing!
S25 Week 3 Study Plan (Hematology, Oncology, Skin, MS, Sensory, Mental Health, Pharm)
Concepts Covered:
- Test Taking Strategies
- EENT Disorders
- Prefixes
- Suffixes
- Disorders of the Adrenal Gland
- Integumentary Disorders
- Bipolar Disorders
- Disorders of the Posterior Pituitary Gland
- Hematologic Disorders
- Immunological Disorders
- Medication Administration
- Musculoskeletal Disorders
- Labor Complications
- Musculoskeletal Trauma
- Disorders of the Thyroid & Parathyroid Glands
- Integumentary Important Points
- Learning Pharmacology
- Anxiety Disorders
- Disorders of Pancreas
- Trauma-Stress Disorders
- Oncology Disorders
- Somatoform Disorders
- Dosage Calculations
- Depressive Disorders
- Personality Disorders
- Cognitive Disorders
- Eating Disorders
- Substance Abuse Disorders
- Psychological Emergencies
- Liver & Gallbladder Disorders
- Upper GI Disorders
- Urinary System
- Cardiac Disorders
- Cardiovascular Disorders
- Female Reproductive Disorders
- Neurologic and Cognitive Disorders
- Shock
- Respiratory Disorders
- Nervous System
- Urinary Disorders
- Pregnancy Risks
- Psychotic Disorders

