Nursing Care Plan (NCP) for Cholecystitis
Included In This Lesson
Study Tools For Nursing Care Plan (NCP) for Cholecystitis
Outline
Lesson Objective for Cholecystitis Nursing Care Plan (NCP):
- Understanding Cholecystitis:
- Define and comprehend the pathophysiology of cholecystitis, including the inflammation of the gallbladder and its impact on digestive processes.
- Identifying Etiological Factors:
- Recognize the key etiological factors contributing to cholecystitis, such as gallstones, infection, or other conditions affecting the gallbladder.
- Desired Outcome Clarification:
- Establish clear expectations for the desired outcomes of nursing interventions, focusing on pain management, prevention of complications, and improvement in overall gallbladder function.
- Comprehensive Nursing Assessment:
- Develop proficiency in conducting a thorough nursing assessment for individuals with cholecystitis, encompassing both subjective and objective data to guide personalized care.
- Effective Implementation and Evaluation:
- Implement and evaluate nursing interventions aimed at managing cholecystitis, considering factors like pain relief, dietary modifications, and patient education to enhance recovery and prevent recurrence.
Pathophysiology of Cholecystitis
- Gallbladder Inflammation:
- Cholecystitis is characterized by inflammation of the gallbladder, often triggered by the accumulation of bile or the presence of gallstones. Inflammation may impede the normal flow of bile.
- Obstruction of Cystic Duct:
- Gallstones can obstruct the cystic duct, preventing the release of bile into the digestive system. This obstruction leads to an accumulation of bile within the gallbladder.
- Ischemia and Tissue Damage:
- Prolonged obstruction and inflammation can cause ischemia (reduced blood flow) to the gallbladder tissues, leading to cellular damage and compromising the organ’s function.
- Bacterial Infection:
- Stagnant bile provides an ideal environment for bacterial overgrowth. Infections can further exacerbate inflammation and contribute to the symptoms associated with cholecystitis.
- Complications and Secondary Inflammation:
- If left untreated, cholecystitis can progress to complications such as gangrene, perforation of the gallbladder, or the development of abscesses, leading to more severe consequences.
Etiology of Cholecystitis
- Gallstones (Cholelithiasis):
- The most common cause of cholecystitis is the presence of gallstones in the gallbladder, obstructing the normal flow of bile and initiating the inflammatory process.
- Infection:
- Bacterial infections, often stemming from bile stasis, contribute to the inflammation of the gallbladder, particularly in cases where there is an obstruction.
- Biliary Stasis:
- Conditions that impede the regular emptying of the gallbladder, such as reduced motility or dysfunction of the gallbladder, can lead to the accumulation of bile and increase the risk of cholecystitis.
- Trauma or Injury:
- Physical trauma to the abdomen or injury to the gallbladder can predispose individuals to cholecystitis by disrupting the normal anatomy and function of the gallbladder.
- Metabolic Factors:
- Certain metabolic factors, such as obesity, rapid weight loss, or diabetes, are associated with an increased risk of gallstone formation, thereby contributing to the development of cholecystitis.
Desired Outcome of Nursing Care for Cholecystitis
- Pain Management:
- Alleviate and control abdominal pain associated with cholecystitis, enhancing the patient’s comfort and overall well-being.
- Inflammation Reduction:
- Decrease inflammation of the gallbladder to promote healing and prevent complications, aiming for normalized gallbladder function.
- Prevention of Complications:
- Prevent the development of complications such as infection, abscess formation, or perforation, ensuring a smoother recovery process.
- Patient Education:
- Educate the patient on dietary modifications, lifestyle changes, and the importance of adherence to prescribed medications to prevent recurrence and promote long-term gallbladder health.
- Improved Quality of Life:
- Enhance the patient’s overall quality of life by addressing symptoms, preventing complications, and empowering the individual to manage their condition effectively.
Cholecystitis Nursing Care Plan
Subjective Data:
- Nausea
- Loss of appetite
- Severe abdominal pain, RUQ or center
Objective Data:
- Fever
- Vomiting
- Jaundice (severe cases)
- Abnormal labs
- Clay-colored stools
Nursing Assessment for Cholecystitis
- Pain Assessment:
- Evaluate the location, intensity, and characteristics of abdominal pain, including factors that aggravate or alleviate the pain.
- Symptom Review:
- Assess for associated symptoms such as nausea, vomiting, indigestion, and changes in bowel habits to gain a comprehensive understanding of the patient’s condition.
- Physical Examination:
- Perform a thorough abdominal examination, checking for tenderness, guarding, and distension. Assess vital signs and signs of systemic infection.
- Dietary History:
- Obtain a detailed dietary history to identify potential triggers and aggravating factors related to the development of cholecystitis, especially in relation to high-fat meals.
- Medical History:
- Review the patient’s medical history, focusing on risk factors such as obesity, diabetes, and previous gallbladder issues.
- Laboratory Tests:
- Order and interpret laboratory tests, including liver function tests and imaging studies like ultrasound, to confirm the diagnosis and assess the severity of cholecystitis.
- Psychosocial Assessment:
- Evaluate the patient’s emotional and psychological well-being, addressing concerns related to pain, anxiety, and potential lifestyle changes associated with the condition.
- Medication Review:
- Review the patient’s current medications, including analgesics and antimicrobials, ensuring appropriate drug therapy for pain management and infection control.
Implementation of Nursing Care for Cholecystitis:
- Pain Management:
- Administer prescribed analgesics as ordered and monitor the patient’s response to pain relief, adjusting medications as needed.
- Implement interventions to reduce inflammation, such as applying heat therapy or administering anti-inflammatory medications as ordered.
- Infection Control:
- Administer antimicrobial medications as prescribed, ensuring completion of the full course to address infection. Monitor for signs of improvement or complications.
- Dietary Guidance:
- Collaborate with a dietitian to develop a low-fat diet plan tailored to the patient’s needs. Educate the patient on dietary modifications to prevent gallbladder irritation.
- Health Promotion:
- Provide health education on lifestyle modifications, including weight management, regular exercise, and the importance of maintaining a balanced diet for overall gallbladder health.
- Prepare for surgery, if indicated
- Cholecystectomy can be performed urgently or as a scheduled procedure for cholecystitis. Educate the patient and prepare them for surgery, including implementing pre-operative labs, NPO status, and consent.
Nursing Interventions and Rationales
- Assess vital signs
Monitor for signs of cardiopulmonary stress and signs of infection
- Tachycardia
- Fever
- Assess Gastrointestinal status
- Look– for distention
- Listen– for frequent belching
- Feel– for abdominal rigidity and palpable gallbladder, note tenderness
- Initiate IV access and administer fluids
- Assess and manage pain
Severe pain is the most common and worrisome symptom. Patients may report pain that radiates from the RUQ to the back
- Administer medications
- Assist with positioning, place in semi-Fowler’s following meals to aid in digestion
- Promote bedrest for comfort
- Administer medications
- Monitor for effectiveness
- Monitor for side effects / adverse reactions
- Antibiotics (levofloxacin, cephalosporins, metronidazole) – in cases of infection and for prophylaxis during surgery or procedures
- Antiemetics (ondansetron, promethazine) – to control nausea and prevent electrolyte imbalances
- Analgesics (oxycodone, acetaminophen)- to manage pain
- Cholecystokinin may be given to prevent gallbladder sludge in patients receiving TPN
- Monitor diagnostic testing
- Labs
- Imaging (Ultrasound, CT, MRI, x-rays)
Labs: labs may not always be reliable, but the following are often noted:
- AST/ALT – may be elevated due to liver dysfunction in cases of obstruction
- Elevated bilirubin may indicate common bile duct obstruction/liver dysfunction
- Urinalysis- can be used to rule out pyelonephritis and renal calculi as a source of pain
- A pregnancy test should be done on all women of childbearing age to prevent the fetal demise
Imaging: Ultrasound is the diagnostic choice as it allows visualization of acute disease without excessive radiation exposure

- Ultrasound
- CT, MRI- may be done for more detailed evaluation or when ultrasound is inconclusive
- Prepare the patient for diagnostic procedures:
- ERCP (Endoscopic Retrograde Cholangiopancreatography) – allows visualization of the biliary system to help diagnose and treat problems with the bile and pancreatic ducts.
- HIDA scan (Hepatobiliary Iminodiacetic Acid)- performed by injecting a radioactive dye into the bloodstream and visualizing the flow through a special camera placed on the abdomen
- Place patient on clear liquids only for 6-12 hours prior to the procedure
- Withhold NSAIDs and anticoagulants prior to the procedure to avoid excess bleeding and interference with the test
- Assist patient with ambulation after the tests as medication (often morphine) given during the procedure may cause drowsiness
- Nutrition and Lifestyle education
- Obesity is often related to gallbladder disease- encourage diet and exercise to control weight
- Avoid foods high in fat such as pork, gravies, fried foods, butter
- Avoid gas-producing foods such as cabbage, beans, carbonated drinks
- Limit or avoid gastric irritants such as alcohol, coffee, tea, caffeine
Evaluation of Nursing Care for Cholecystitis
- Pain Relief Assessment:
- Evaluate the effectiveness of pain management interventions by assessing the patient’s pain levels regularly. Adjust pain management strategies based on the patient’s feedback.
- Resolution of Inflammation:
- Monitor laboratory results and clinical indicators to assess the resolution of inflammation. Evaluate the effectiveness of anti-inflammatory measures in promoting gallbladder healing.
- Absence of Complications:
- Monitor for and assess the absence or reduction of complications such as infection, abscess formation, or perforation, ensuring timely intervention if complications arise.
- Dietary Adherence:
- Assess the patient’s adherence to dietary recommendations, providing reinforcement and clarification as needed. Evaluate the impact of dietary changes on symptoms and overall well-being.
- Patient Education Outcomes:
- Evaluate the patient’s understanding of the condition, treatment plan, and preventive measures. Measure the patient’s ability to manage their health and make informed decisions related to gallbladder care.
References
- https://www.mayoclinic.org/diseases-conditions/cholecystitis/symptoms-causes/syc-20364867
- https://www.webmd.com/digestive-disorders/what-is-chloecystitis#1
- https://emedicine.medscape.com/article/171886-overview
- https://www.niddk.nih.gov/health-information/diagnostic-tests/endoscopic-retrograde-cholangiopancreatography
- https://www.webmd.com/digestive-disorders/what-is-gallbladder-scan#1
Example Nursing Diagnosis For Nursing Care Plan (NCP) for Cholecystitis
- Acute Pain: Cholecystitis often causes severe abdominal pain. This diagnosis addresses the pain management needs of the patient.
- Risk for Infection: Cholecystitis can lead to infection or abscess formation. This diagnosis emphasizes infection prevention.
- Imbalanced Nutrition: Less than Body Requirements: Cholecystitis may affect the patient’s ability to tolerate and digest food. This diagnosis addresses nutritional deficits.
Transcript
Hey guys, in this care plan, we will explore Cholecystitis.
So, in this Cholecystitis care plan, we’re going to talk about the desired outcome of our patient, the subjective and objective data, along with the nursing interventions and rationale for each SAR, medical diagnosis is Cholecystitis.
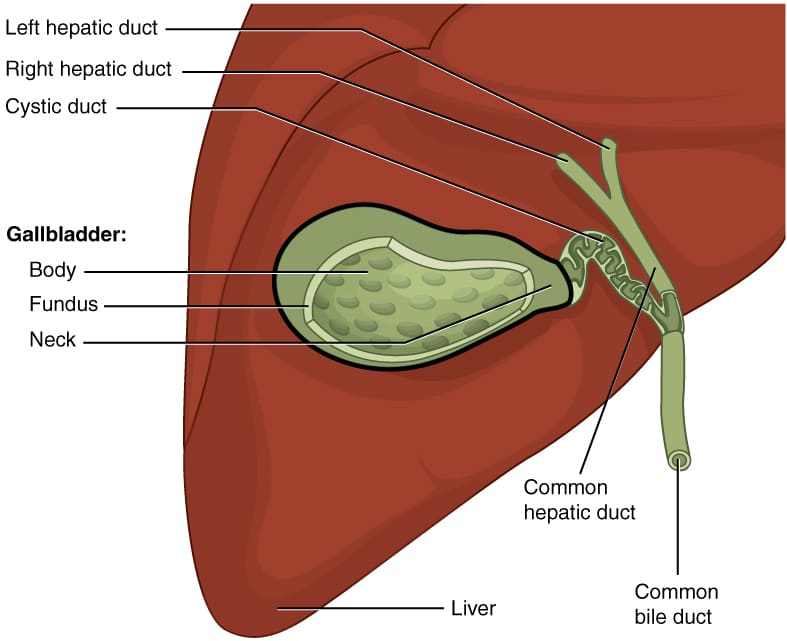
So, Cholecystitis is inflammation of the gallbladder, which holds bile that is actually released into the small intestines. So, let’s imagine this is our small intestines here. So, when that bile duct between the gallbladder and the small intestines gets blocked, the bile becomes trapped causing that inflammation in the gallbladder. The obstruction of the bile duct causes inflammation and it could be caused by gallstones, biliary, sludge infections, tumors, or blood vessel compression. So, the desired outcome of our patient is that they’ll be free from pain and resume and maintain optimal diet and nutrition.
Now, let’s look at our care plan. So, the patient may be experiencing some nausea and loss of appetite because of the blockage that isn’t allowing the bile to flow into the intestines. So, the patient may be experiencing severe abdominal pain in the right upper quadrant or in the center because of the blockage and inflammation.
Now, let’s look at our objective data. So, the inflammation of the gallbladder might cause your patient to have a fever. Your patient may begin vomiting due to the blockage of the bile. The patient may have abnormal lab values like their liver enzymes because the liver is what creates the bile that then travels through the bile duct into the gallbladder. So, when Cholecystitis progresses and the tissue begins to die, the liver becomes more affected resulting in those elevated liver enzymes and even sometimes jaundice. So, Bilirubin may be elevated indicating bile duct obstruction as well. The patient might have clay colored stool because of the lack of bile to change the color of the stool to brown.
Now, let’s look at our nursing interventions in the rationales. So, our first nursing intervention is to assess your patient’s vital signs. Look for tachycardia and fevers, because that could indicate infection in your patient. Next, you will assess the gastrointestinal status of your patient. Look for abdominal distension, listen for belching and feel for abdominal rigidity.
Our next nursing intervention is to assess and manage your patient’s pain. The inflammation and obstruction causes pain that might radiate to the back. Next, you administer medications for the patient, such as antibiotics for infections, analgesics for pain, antiemetics for nausea and vomiting, and IV fluids to help hydrate your patient while they’re resting their bowels. Be sure to monitor the diagnostic testing of your patient. Look at those lab values in the imaging to view the gallbladder and how it’s doing. So, you will prepare for any procedures that they might have. The patient might be on a clear liquid diet prior, and you will have to withhold any anticoagulants and NSAIDS to avoid bleeding.
Our last nursing intervention is to provide nutrition and lifestyle education, encourage a low fat diet because it’s easier to digest and avoid gastric irritants because they could worsen diarrhea. The diarrhea after gallbladder removal occurs because of the direct drainage of the bile into the intestine from the liver. It no longer will have the gallbladder to rest in. It’s going to go straight into the intestines causing diarrhea.
We love you guys. Now go out and be your best self today and as always, happy nursing!
